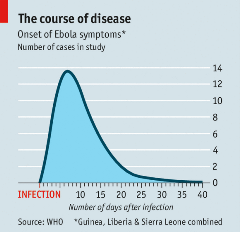
If you hadn’t heard of Ebola virus prior to the 2014-2016 outbreak, you are not alone. However, the world has experienced over twenty documented outbreaks of this hemorrhagic fever disease, most of which have occurred in Africa.1 Ebola virus disease is severe and often fatal if untreated, with an average fatality rate of 50%. The virus is believed to most often originate from contact with an infected wild animal, and spreads human-to-human through contact with bodily fluids.2 Symptoms can take up to 21 days to develop (see image below).2,20
Quick response and successful vaccination allowed for better containment of the May 2018 outbreak in the Équateur Province of the Democratic Republic of Congo (DRC). Within two months, the World Health Organization (WHO) and partners had treated the last confirmed case and were ready to begin a 42 day wait (two incubation periods) before officially declaring it over.3
Unfortunately, just one week after the government declared this outbreak over, a new outbreak was confirmed in another part of the DRC, relaunching response efforts.
Although the vaccine used in the Équateur outbreak was crucial in containment, it is still in experimental trials and research continues for additional prevention techniques and treatments for the various strains of Ebola virus.
Recent outbreaks
The world was stunned when the 2014-2016 Ebola outbreak infected over 28,000 people and resulted in at least 11,000 deaths. Although this outbreak was concentrated in countries of Africa, nations throughout the world took precautions to monitor for potential cases. As international travel becomes more prevalent, the risk of spreading disease from country to country is elevated, and despite these efforts, seven other countries saw cases of Ebola during this outbreak.4 According to the Centers for Disease Control (CDC), “Weak surveillance systems and poor public health infrastructure contributed to the difficulty surrounding the containment of this outbreak”.4
In contrast, the Équateur outbreak garnered much swifter action and better containment. Of particular concern in this outbreak was the spread to urban areas where disease can proliferate much more quickly due to closer proximity than rural areas. The WHO and its partners quickly intervened to set up treatment centers and distribute an experimental vaccine to people who had come in contact with the virus and their contacts. 5 These efforts limited the outbreak to 53 cases and 29 deaths.
Just one week after the previous outbreak was declared over, 26 cases of hemorrhagic-like fevers and 20 deaths were reported to the government from the North Kivu and Ituri provinces.6 Six samples were analyzed, and four tested positive for Ebola.6 Fortunately, staff and equipment are still in the DRC from the last outbreak so they can quickly respond to the new one. However, this outbreak poses its own challenges. It may be more difficult to reach contacts as this outbreak is in an active conflict zone where many are hiding from or serving in militias, raising concerns for personnel safety.7 In addition, the staff have yet to confirm the strain of this new outbreak. If it’s different than the previous strain, it is unknown if the same vaccine will be effective.6

Lessons from Disaster
After the 2014-2016 outbreak, researchers resumed testing the vaccine deployed in Équateur. Gavi, the vaccine alliance, had 300,000 doses stored in 2016 in case of another outbreak.8 These actions made a quick response possible in 2018. One concern with transporting vaccines is the lack of electrical stability in Africa, making the required refrigeration challenging. Backed by the Global Good program, a collaboration between Bill Gates and Intellectual Ventures, Arktek™ was developed.9 Arktek™ is a cooler which uses vacuum insulation between double walls and reinforced fiberglass.8 This cooler can keep vaccines at the proper temperature for at least one month, allowing workers to transport them to remote locations.9
In the aftermath of the Équateur outbreak, new surveillance and community education initiatives have been deployed in hopes of reducing the impact of future outbreaks. The DRC’s Ministry of Health is partnering with the WHO to create a plan for outbreak survivors in which counseling and additional screening can be completed.5 In addition, initiatives for “risk communication, social mobilization and community engagement activities continue in the area with support for active community-based alerts for epidemic prone diseases, addressing rumors related to Ebola virus disease and reduction of stigma against survivors”.5
Research continues
Although the vaccine proved instrumental in reducing spread in the May outbreak, research continues to advance the development of potential prevention techniques, therapeutics, and more advanced vaccines.
Measurement of body temperature has long been considered the standard marker for models of febrile disease, and has been used to assess both vaccine and therapeutic treatments for Ebola virus.10,11,12 In the development of several models, including both intramuscular and respiratory exposure to virus, more advanced physiological parameters such as blood pressure (BP), left ventricular pressure (LVP), heart rate (HR) and electrocardiogram (ECG) have been monitored.13,14,15 In Ebola virus research, these parameters are most often studied in primates as their experiences of symptoms, pathogenesis, and outcomes are very similar to those experienced by humans.16 Other species used include rodents, hamsters, and guinea pigs.16
It is believed glucose could be another potential biomarker for severe disease progression in models. Although downward trends in glucose were identified in a statistical evaluation of Ebola virus-exposed animals, the potential variability of glucose analysis from serum due to processing or timing was a concern.17 The use of continuous blood glucose monitoring could aid further understanding.
The value of using temperature and additional physiological parameters was highlighted by researchers who utilized DSI telemetry during the development of a pre-symptomatic detection tool. The goal of this study was to utilize telemetry data to develop a machine-learning algorithm that could indicate pathogen exposure as soon as possible, using only physiological data.18 By detecting exposure during earlier asymptomatic stages, researchers and clinicians would have more time to perform advanced diagnostics, provide earlier treatment and potentially minimize the spread of an outbreak.18
Advancing Ebola research
DSI has solutions for Ebola researchers, ranging in size from mouse to primate, which can be used to develop models of the virus, identify biomarkers, and to evaluate virus effects and treatment options.
Animal Model Development
Plethysmography methods including head out and Jacketed External Telemetry (JET) with respiratory inductive plethysmography (RIP) can be used to expose animals to Ebola virus. 19
DSI’s temperature monitoring solutions can then be used to ensure infection has taken, indicating a successful animal model is created.
Biomarker Identification
Temperature is the most well-known biomarker of hemorrhagic disease. DSI’s PhysioTel™ line of implantable telemetry includes options for measuring temperature alone, or in combination with other endpoints.
DSI also created the first solution for monitoring second-to-second blood glucose in freely moving animals which can be used to help discover new biomarkers, as glucose is thought to have potential.
Evaluating Effects of Ebola and Treatment Effectiveness
Some researchers may also need to measure the virus’ effects on blood pressure, cardiac function, or respiration. DSI offers the widest range of physiologic signal monitoring options for animal models, offering solutions to measure these endpoints and more with the PhysioTel™ telemetry and Buxco® respiratory products.
If you are interested in learning more about DSI’s solutions for Ebola research, please complete our form to receive further information.
References
1Centers for Disease Control. (2018). “Years of Ebola Virus Disease Outbreaks”. https://www.cdc.gov/vhf/ebola/history/chronology.html
2World Health Organization. (2018). “Ebola virus disease”. http://www.who.int/news-room/fact-sheets/detail/ebola-virus-disease
3Bearak, M. (2018). “We Have Some Great News About The Ebola Outbreak in Congo”. The Washington Post. https://www.washingtonpost.com/news/worldviews/wp/2018/06/27/remember-that-ebola-outbreak-in-congo-looks-like-they-contained-it/?noredirect=on&utm_term=.60fa066e1e42
4Centers for Disease Control. (2017). “2014-2016 Ebola Outbreak in West Africa”. https://www.cdc.gov/vhf/ebola/history/2014-2016-outbreak/index.html
5World Health Organization. (2018). “Ebola virus disease – Democratic Republic of the Congo: Disease outbreak news, 6 July 2018”. Relief Web. https://reliefweb.int/report/democratic-republic-congo/ebola-virus-disease-democratic-republic-congo-disease-outbreak-7
6Weber L. (2018). “New Ebola Outbreak Confirmed In Democratic Republic of Congo”. Huffpost. https://www.huffingtonpost.com/entry/ebola-democratic-republic-congo_us_5b61d252e4b0fd5c73d56d92
7World Health Organization. (2018). “Cluster of presumptive Ebola cases in North Kivu in the Democratic Republic of the Congo”. http://www.who.int/news-room/detail/01-08-2018-cluster-of-presumptive-ebola-cases-in-north-kivu-in-the-democratic-republic-of-the-congo
8Rogers A. (2018). “The Wild Logistical Ride of the Ebola Vaccine’s High-tech Thermos”. Wired. https://www.wired.com/story/the-wild-logistical-ride-of-the-ebola-vaccines-high-tech-thermos/
9Intellectual Ventures. (2018). “Passive Vaccine Storage Device”. http://www.intellectualventures.com/inventions-patents/our-inventions/vaccine-cold-chain-device/
10Pettitt J, Zeitlin L, Kim DH, Working C, Johnson JC, Bohorov O, Bratcher B, Hiatt E, Hume SD, Johnson AK, Morton J, Pauly MH, Whaley KJ, Ingram MF, Zovanyi A, Heinrich M, Piper A, Zelko J, Olinger GG. (2013). “Therapeutic intervention of Ebola virus infection in rhesus macaques with the MB-003 monoclonal antibody cocktail”. Sci Transl Med. 5(199):199ra113. doi: 10.1126/scitranslmed.3006608. http://stm.sciencemag.org/content/5/199/199ra113
11Trefry JC, Wollen SE, Nasar F, Shamblin JD, Kern SJ, Bearss JJ, Jefferson MA, Chance TB, Kugelman JR, Ladner JT, Honko AN, Kobs DJ, Wending MQ, Sabourin CL, Pratt WD, Palacios GF, Pitt ML. (2015). “Ebola Virus Infections in Nonhuman Primates Are Temporally Influenced by Glycoprotein Poly-U Editing Site Populations in the Exposure Material”. Viruses. 7(12):6739-54. doi: 10.3390/v7122969. http://www.mdpi.com/1999-4915/7/12/2969
12Pascal KE, Dudgeon D, Trefry JC, Anantpadma M, Sakurai Y, Murin CD, Turner HL, Fairhurst J, Torres M, Rafique A, Yan Y, Badithe A, Yu K, Potocky T, Bixler SL, Chance TB, Pratt WD, Rossi FD, Shamblin JD, Wollen SE, Zelko JM, Carrion R Jr, Worwa G, Staples HM, Burakov D, Babb R, Chen G, Martin J, Huang TT, Erlandson K, Willis MS, Armstrong K, Dreier TM, Ward AB, Davey RA, Pitt MLM, Lipsich L, Mason P, Olson W, Stahl N, Kyratsous CA. (2018). “Development of clinical-stage human monoclonal antibodies that treat advanced Ebola virus disease in non-human primates”. J Infect Dis. doi: 10.1093/infdis/jiy285. https://academic.oup.com/jid/advance-article/doi/10.1093/infdis/jiy285/5025816
13Twenhafel NA, Mattix ME, Johnson JC, Robinson CG, Pratt WD, Cashman KA, Wahl-Jensen V, Terry C, Olinger GG, Hensley LE, Honko AN. (2013). “Pathology of experimental aerosol Zaire ebolavirus infection in rhesus macaques”. Vet Pathol. 50(3):514-29. doi: 10.1177/0300985812469636. http://journals.sagepub.com/doi/abs/10.1177/0300985812469636?url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&rfr_dat=cr_pub%3Dpubmed&
14Kortepeter MG, Lawler JV, Honko A, Bray M, Johnson JC, Purcell BK, Olinger GG, Rivard R, Hepburn MJ, Hensley LE. (2011). “Real-time monitoring of cardiovascular function in rhesus macaques infected with Zaire ebolavirus”. J Infect Dis. 204 Suppl 3:S1000-10. doi: 10.1093/infdis/jir337. https://academic.oup.com/jid/article/204/suppl_3/S1000/2192757
15Zumbrun EE, Bloomfield HA, Dye JM, Hunter TC, Dabisch PA, Garza NL, Bramel NR, Baker RJ, Williams RD, Nichols DK, Nalca A. (2012). “A characterization of aerosolized Sudan virus infection in African green monkeys, cynomolgus macaques, and rhesus macaques”. Viruses. 4(10):2115-36. doi: 10.3390/v4102115. http://www.mdpi.com/1999-4915/4/10/2115
16St Claire MC, Ragland DR, Bollinger L, Jahrling PB. (2017). “Animal Models of Ebolavirus Infection”. Comp Med. 67(3): 253–262. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5482517/
17Warren TK, Trefry JC, Marko ST, Chance TB, Wells JB, Pratt WD, Johnson JC, Mucker EM, Norris SL, Chappell M, Dye JM, Honko AN. (2014). “Euthanasia assessment in ebola virus infected nonhuman primates”. Viruses.6(11):4666-82. doi: 10.3390/v6114666. http://www.mdpi.com/1999-4915/6/11/4666/htm
18Milechin L, Davis S, Patel T, Hernandez M, Ciccarelli G, Schwartz S, Samsi S, Hensley L, Goff A, Trefry J, Johnston S, Purcell B, Cabrera C, Fleischman J, Reuther A, Rossi F, Honko A, Pratt W, Swiston Jr. A. (2017). “Detecting pathogen exposure during the non-symptomatic incubation period using physiological data”. bioRxiv. https://doi.org/10.1101/218818
19Bohannon JK, Honko AN, Reeder RJ, Cooper K, Byrum R, Bollinger L, Kuhn JH, Wada J, Qin J, Jahrling PB, Lackemeyer MG. (2016). “Comparison of respiratory inductive plethysmography versus head-out plethysmography for anesthetized nonhuman primates in an animal biosafety level 4 facility”. Inhal Toxicol. 28(14):670-676. https://www.tandfonline.com/doi/abs/10.1080/08958378.2016.1247199
20The Economist. (2014). “A killer in close up”. https://www.economist.com/international/2014/10/16/a-killer-in-close-up